Patients are becoming more and more involved in the clinical decision making process, but how does this work and what are the benefits?
In many countries, patients are actively involved in their own medical care, with medical decisions made in partnership with clinicians. This can help avoid patient dissatisfaction with the decision-making process about their treatment options and decrease the risk of complaints or claims against a doctor.
The inclusion of patients in the decision-making process does vary among the different healthcare systems, where regulations and culture often dictate a more traditional paternalistic decision-making model.
However, as society becomes more educated and interconnected, and as patients become more aware of the medical and technological advances, a shift to involve patients in their own medical care is becoming more and more common.
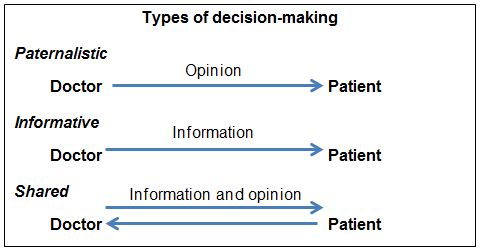
Neither a paternalistic model of “doctor knows best” nor an informative approach of “here’s all the information, you decide” are likely to satisfy most patients. These two styles are different from making the decision in partnership with the patient, where there is an exchange of knowledge and opinion (See Box 1).
Box 1:
The patient’s preference
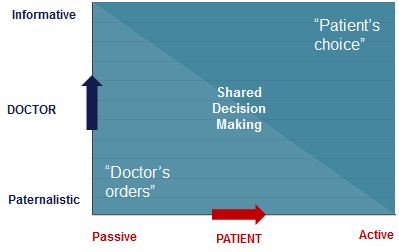
Resistance to shared decision-making often revolves around a perception that doctors have many patients who wish the doctor to make the decision for them. The difficulty is that just as doctors have preferences for their style of decision-making, patients also have preferences as to their desired level of involvement (see figure 1).
Figure 1:
Doctors’ recommendations
Consider these three approaches in the context of a 26-year-old female patient with a young daughter who is requesting contraception as she has started a new relationship:
Scenario A: Paternalistic
Doctor: We find that most women in your situation choose a coil and that’s what I would recommend for you. Let me tell you about the risks and benefits…
Scenario B: Informative
Doctor: There are lots of choices available. I have a comprehensive information booklet here about all the options and their risks and benefits. Why don’t you have a good look at that and let me know which you would prefer?
Scenario C: Shared decision-making
Doctor: What matters to you most about the choice of contraception? Is it reliability, minimal side effects, impact on your bleeding pattern or something else?
Patient: The most important thing for me, doctor, is not to get pregnant so early in a new relationship, so I would like the most reliable method.
Doctor: There are several options, including… "Given that not becoming pregnant is your most important consideration, I would probably recommend the combined pill, assuming there aren’t any contraindications. What do you know about the pill?"
The doctor’s recommendation is a vital ingredient to help arrive at the decision but may be invalid unless based on patient preferences, concerns, values and expectations.
Patient dissatisfaction
Most dissatisfaction with clinical decision-making relates to:
- The amount and quality of information received
- Level of involvement in the decision-making process.
Numerous studies have shown that doctors’ assumptions of patient values on which they may base their recommendations regarding investigation or treatment can be inaccurate.3 Better-informed patients often make different choices as what patients want is often different from what doctors think their patients want.
Often clinicians decide what they think is in the patient’s best interest from a clinical perspective, inform them as to why they have arrived at that decision and then give them details of the risks and benefits. This represents more persuasion than collaboration, acquiescence rather than concordance or making decisions for rather thanwith the patient. The danger is that clinicians could subject patients to operations, investigations or medications that they don’t want.5
Shared decision-making has significant benefits (see Box 2) and should be an integral part of interactions with patients. The initial consultation may take a little longer but less than the time spent dealing with uncertain or unhappy patients.1,4
Box 2:
Our local knowledge and expertise are unrivalled. We’ve been protecting doctors in Hong Kong for over 60 years. Join Medical Protection in order to request advice and legal representation for coroner inquests, disciplinary and regulatory proceedings and criminal investigations related to your professional practice today.
References
1Coulter A, Collins A, Making shared decision making a reality, No decision about me, without me. London: King’s Fund (2011)
2The Health Foundation, Helping people share decision making, London: The Health Foundation (2012)
3Stacey D et al, Decision aids for people facing health treatment or screening options, Cochrane Database Syst Rev 10: CD001431 (2011)
4Kennedy A et al, Effect of decision aids for menorrhagia on treatment choices, health outcomes and cost: a randomised controlled trial, JAMA 288:2701-8 (2002)
5Mulley et al, Patient preferences matter: stop the silent misdiagnosis, King’s Fund (2012)